Corona Virus || COVID -19 Protection and Treatment
1.1 Layout
(1)
Healthcare
facilities shall found out a comparatively independent fever clinic including
an exclusive one-way passage at the doorway of the hospital with a clear sign;
(2)
The
movement of individuals shall follow the principle of "three zones and two
passages" : a contaminated zone, a potentially contaminated zone and a
clean zone provided and clearly demarcated, and two buffer zones between the
contaminated zone and the potentially contaminated zone;
(3)
An
independent passage shall be equipped for contaminated items; found out a
visible region for one-way delivery of things from an office area (potentially
contaminated zone) to an isolation
ward (contaminated zone);
(4)
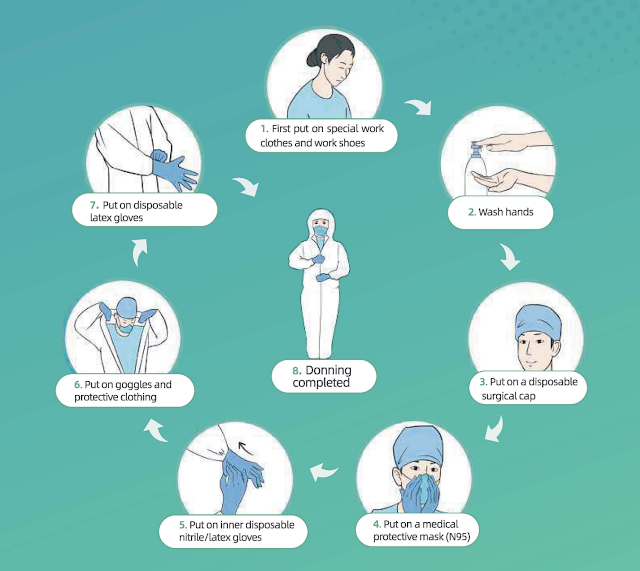
Appropriate
procedures shall be standardized for medical personnel to put on and take off
their protective equipment. Make flowcharts of different zones, provide
full-length mirrors and observe the walking routes strictly;
(5)
Infection prevention and control technicians
shall be assigned to supervise the medical personnel on putting on and removing
protective equipment so on prevent contamination;
(6)
All items
in the contaminated zone that have not been disinfected shall not be removed.
1.2
Zone Arrangement
(1) Found
out an independent examination room, a laboratory, an
observation room, and a resuscitation room;(2) Found out a per-examination and triage area to perform preliminary screening of patients;
(3) Separate diagnosis and Treatment of Corona Virus Affected zones: those patients with an epidemiological history and fever and/or respiratory symptoms shall be guided into a suspected COVID-19 / CORONA VIRUS AFFECTED patient zone; those patients with regular fever but no clear epidemiological history shall be guided into a daily fever patient zone.
1.3 Patient Management
(1) Patients with fevers must wear medical surgical masks;(2) Only patients are allowed to enter the lounge so as to avoid overcrowding;
(3) The duration of the patient's visit shall be minimized so on avoid cross infections;
(4) Educate patients and their families about early identification of symptoms and essential preventative actions.
1.4 Screening, Admission and Exclusion
1.4.1 All healthcare workers shall fully
understand the epidemiological and clinical features of COVID-19 / CORONA VIRUS AFFECTED and screen patients in accordance with the
screening criteria below (see Table 1);
1.4.2
Macromolecule testing (NAT) shall be
conducted on those patients who meet the screening criteria for suspected
patients;
1.4.3
Patients who don't meet the screening
criteria above, if they are doing not have a confirmed epidemiological history,
but cannot be ruled out from having COVID-19
/ CORONA VIRUS AFFECTED supported
their symptoms, especially through imaging, are recommended for further
evaluation and to urge a comprehensive diagnosis;
1.4.4
Any patient who tests negative shall be
re-tested 24 hours later. If a patient has two negative NAT results and
negative clinical manifestations, then he or she is going to be ruled out from
having COVID-19 / CORONA VIRUS AFFECTED and
discharged from the hospital. If those patients can't be ruled out from having COVID-19 / CORONA VIRUS AFFECTED infections supported their clinical
manifestations, they shall be subjected to additional NAT tests every 24 hours
until they're excluded or confirmed;
1.4.5
Those confirmed cases with a positive
NAT result shall be admitted and treated collectively based on the severity of
their conditions (the general isolation
ward or isolated ICU).
 |
Table 1: Corona Virus || COVID -19 Protection and Treatment |
1.1
Isolation
Ward Area
1.2 Scope of Application
The isolation ward area includes an observation ward area, isolation wards, and an isolation ICU area. The building layout and workflow shall meet the relevant requirements of the hospital isolation technical regulations. Medical providers with negative pressure rooms shall implement standardized management in accordance with relevant requirements.Strictly limit access to isolation wards.
1.3 Layout
Please ask fever clinic.1.4 Ward Requirements
(1) Suspected and confirmed patients shall be separated in several ward areas;(2) Suspected patients shall be isolated in separated single rooms. Each room shall be equipped with facilities like a personal bathroom and therefore the patient's activity should be confined to the isolation ward;
(3) Confirmed patients are often arranged within the same room with bed spacing of not but
COVID-19 Animation: What Happens If You Get Corona virus?
1.5
1.2 meters (appx 4 feet). the space shall
be equipped with facilities like a toilet and the patient's activity must be
confined to the isolation ward.
1.6 Patient Management
(1) Family visits and nursing shall be declined. Patients should be allowed to possess their electronic communication devices to facilitate interactions with loved ones;(2) Educate patients to assist them prevent further spread of C0VID-19, and supply instructions on the way to wear surgical masks, proper hand washing, cough etiquette, medical observation and residential quarantine.
1.1 Staff Management
1.2 Workflow Management
1.2 .1
Before working during a fever clinic
and isolation ward, the staff must
undergo strict training and examinations to make sure that they skills to place
on and take away personal protective equipment. they need to pass such
examinations before being allowed to figure in these wards.
1.2.2
The staff should be divided into different
teams. Each team should be limited to a maximum of 4 hours of working in an isolation ward. The teams shall add the
isolation wards (contaminated zones)
at different times.
1.2.3
Arrange Treatment of Corona Virus Affected, examination and disinfection for
each team as a gaggle to reduce the frequency of staff occupation and out of
the isolation wards.
1.2.4
Before going off duty, staff must wash
themselves and conduct necessary personal hygiene regimens to prevent possible
infection of their respiratory tracts and mucosa.
 |
Isolation and Treatment forCorona Virus || COVID -19 Protection and Treatment |
1.1
Health Management
1.1.1 The front-line staff within the isolation areas - including healthcare personnel, medical technicians and property & logistics personnel - shall sleep in an isolation accommodation and shall not leave without permission.
1.1.1 The front-line staff within the isolation areas - including healthcare personnel, medical technicians and property & logistics personnel - shall sleep in an isolation accommodation and shall not leave without permission.
1.1.2
A nutritious diet shall be provided to
reinforce the immunity of medical personnel.
1.1.3
Monitor and record the health status of
all staff on the work, and conduct health monitoring for front-line staff,
including monitoring body temperature and respiratory symptoms; help address
any psychological and physiological problems that arise with relevant experts.
1.1.4
If the staff has any relevant symptoms
like fever, they shall be isolated immediately and screened with an NAT.
1.1.5
When the front-line staff including
healthcare personnel, medical technicians and property & logistics
personnel finish their add the isolation
area and are returning to normal life, they shall first be NAT tested for
SARS-CoV-2. If negative, they shall be isolated collectively at a specified
area for 14 days before being discharged from medical observation.
1.1
Disinfection
Procedures for COVID-19 / CORONA VIRUS
AFFECTED Isolation Ward Area
Coronavirus Symptoms, Diagnosis, Treatment, & Vaccine Status|| Corona Virus || COVID -19 Protection and Treatment
1.2 Disinfection for Floor and Walls
1.2.1
Visible
pollutants shall be completely removed before disinfection and handled in accordance
with disposal procedures of blood and liquid body substance spills;
1.2.2
Disinfect
the ground and walls with 1000 mg/L chlorine-containing disinfectant through floor
mopping, spraying or wiping;
1.2.3
Confirm
that disinfection is conducted for a minimum of 30 minutes;
1.2.4
Perform
disinfection 3 times each day and repeat the procedure at any time when there is
contamination.
1.3 Disinfection of Object Surfaces
1.3.1
Visible
pollutants should be completely removed before disinfection and handled in accordance
with disposal procedures of blood and liquid body substance spills;
1.3.2
Wipe the
surfaces of objects with 1000 mg/L chlorine-containing disinfectant or wipes with
effective chlorine; await half-hour then rinse with clean water. Perform
disinfection procedure 3 times each day (repeat at any time when contamination
is suspected);
1.3.3
Wipe
cleaner regions first, then more contaminated regions: first wipe the thing
surfaces that aren't frequently touched, and then wipe the thing surfaces that
are frequently touched. (Once an object surface is cleaned, replace the used
wipe with a replacement one).
1.4 Air Disinfection
1.4.1
Plasma air
sterilizers are often used and continuously run air disinfection in an
environment with human activity;
1.4.2
If there's
no plasma air sterilizers, use ultraviolet lamps for 1 hour whenever. Perform
this operation three times each day.
1.5 Disposal of fecal matter and Sewage
1.5.1
Before
being discharged into the municipal system, fecal matter and sewage must be
disinfected by treating with chlorine-containing disinfectant (for the initial Treatment of Corona Virus Affected ,
the active chlorine must be quite 40 mg/L). Confirm the disinfection time is a
minimum of 1.5 hours;
1.5.2
The
concentration of total residual chlorine within the disinfected sewage should
reach 10 mg/L.
 |
Isolation and Treatment forCorona Virus || COVID -19 Protection and Treatment |
3 Disposal Procedures for Spills of COVID-19 / CORONA VIRUS AFFECTED Patient Blood/Fluids
3.1 For spills of a little volume (< 10 ml) of blood/bodily fluids:
3.1.1
Option 1:
The spills should be covered with chlorine-containing disinfecting wipes
(containing 5000 mg/L effective chlorine) and punctiliously removed, then the
surfaces of the thing should be wiped twice with chlorine-containing
disinfecting wipes (containing 500 mg/L effective chlorine);
3.1.2
Option 2:
Carefully remove the spills with disposable absorbent materials like gauze, wipes,
etc., which are soaked in 5000 mg/L chlorine-containing disinfecting solution.
3.2 For spills of an out sized volume (> 1 O ml) of blood and bodily fluids:
(1)
First, place signs to point the presence of a spill;
(2)
Perform disposal procedures consistent with Option 1 or 2 described below:
Option
1: Absorb the spilled fluids for half-hour with a clean absorbent towel
(containing peroxyacetic acid which will absorb up to 1 L of liquid per towel)
then clean the contaminated area after removing the pollutants.
Option
2: Completely cover the spill with disinfectant powder or bleach powder
containing water-absorbing ingredients or completely cover it with disposable
water-absorbing materials then pour a sufficient amount of 10,000 mg/L
chlorine-containing disinfectant onto the water-absorbing material (or cover
with a dry towel which can be subjected to high-level disinfection). Leave for
a minimum of half-hour before carefully removing the spill.
(3) Fecal
matter, secretions, vomit, etc. from patients shall be collected into special
containers and disinfected for two hours by a 20,000 mg/L chlorine-containing
disinfectant at a spill-to-disinfectant ratio of 1 :2.
(4)
After removing the spills, disinfect the surfaces of the polluted environment
or objects.
(5) The
containers that hold the contaminants are often soaked and disinfected with
5,000 mg/L active chlorine-containing disinfectant for half-hour then cleaned.
(6)
The collected pollutants should be disposed of as medical waste.
(7)
The used items should be put into double-layer medical waste bags and disposed
of as medical waste.
4 Cleaning and Disinfection Procedures for Digestive Endoscopy and Bronchofibroscopy
(1)
Soak the endoscope and reusable valves in 0.23% peroxyacetic acid (confirm the concentration
of the disinfectant before use to form sure it'll be effective);
(2)
Connect the perfusion line of every channel of the endoscope, inject 0.23%
peroxyacetic acid liquid into the road with a 50 ml syringe until fully filled,
and await 5 minutes;
(3) Detach
the perfusion line and wash each cavity and valve of the endoscope with a disposable
special cleaning brush;
(4)
Put the valves into an ultrasonic oscillator containing enzyme to oscillate it.
Connect the perfusion line of every channel with the endoscope. Inject 0.23%
peroxyacetic acid into the road with a 50 ml syringe and flush the road
continuously for five minutes. Inject air to dry it for 1 minute;
(5)
Inject clean water into the road with a 50 ml syringe and flush the road
continuously for 3 minutes. Inject air to dry it for 1 minute;
(6)
Perform a leakage test on the endoscope;
 |
Chloroquine May Fight Covid-19—and Silicon Valley's Into It | WIRED |
(7) Put in an automatic endoscopic washing and disinfection machine. Set a high level of disinfection for Treatment of Corona Virus Affected;
(8)
Send the devices to the disinfection supply center to undergo sterilization
with ethylene oxide.
4.1
Pre-Treatment of Corona Virus Affected of
Other Reusable Medical Devices
(1) If
there are not any visible pollutants, soak the device in 1000 mg/l
chlorine-containing disinfectant for a minimum of 30 minutes;
(2) If
there are any visible pollutants, soak the device in 5000 mg/l
chlorine-containing disinfectant for a minimum of 30 minutes;
(3)
After drying, pack and fully enclose the devices and send them to the
disinfection supply center.
 |
Corona Virus || COVID -19 Protection and Treatment as well as Prevention Related Medical Device |
5.1 Infectious fabrics
(1)
Clothes, bed sheets, bed covers and pillowcases employed by patients;
(2)
Ward area bed curtains;
(3)
Floor towels used for environmental cleaning.
5.2 Collection methods
(1)
First, pack the fabrics into a disposable water-soluble bag and seal the bag
with matching cable ties;
(2)
Then, pack this bag into another bag, seal the bag with cable ties during a
goose neck fashion;
(3) Finally,
pack the bag into a yellow fabric bag and seal the bag with cable ties;
(4)
Attach a special infection label and therefore the department name. Send the
bag to the laundry room.
5.3 Storage and washing
(1)
Infectious fabrics should be separated from other infectious fabrics (non-COVID-19 / CORONA VIRUS AFFECTED) and washed
during a dedicated washing machine;
(2)
Wash and disinfect these fabrics with chlorine-containing disinfectant at 90 °c
for a minimum of 30 minutes.
5.4 Disinfection of
transport tools
(1)
Special transport tools should be used specifically for transporting infectious
fabrics;
(2)
The tools shall be disinfected immediately whenever after getting used for
transporting infectious fabrics;
(3)
The transport tools should be wiped with chlorine-containing disinfectant (with
1000 mg/L active chlorine). Leave disinfectant for half-hour before wiping the
tools clean with clean water.
6 Disposal Procedures for COVID-19 / CORONA VIRUS AFFECTED Related Medical Waste
(1) All waste generated from suspected or confirmed patients shall be disposed
of as medical waste;
(2) Put the medical waste into a double-layer medical waste bag, seal the bag with cable ties during a gooseneck fashion and spray the bag with 10 mg/L chlorine containing disinfectant;
(3) Put sharp objects into a special plastic box, seal the box and spray the box with 10 mg/L chlorine-containing disinfectant;
(4) Put the bagged waste into a medical waste transfer box, attach a special infection label, fully enclose the box and transfer it;
(5) Transfer the waste to a short lived storage point for medical waste along a specified route at a fixed time point and store the waste separately at a fixed location;
(6) The medical waste shall be collected and disposed of by an approved medical waste disposal provider.
(2) Put the medical waste into a double-layer medical waste bag, seal the bag with cable ties during a gooseneck fashion and spray the bag with 10 mg/L chlorine containing disinfectant;
(3) Put sharp objects into a special plastic box, seal the box and spray the box with 10 mg/L chlorine-containing disinfectant;
(4) Put the bagged waste into a medical waste transfer box, attach a special infection label, fully enclose the box and transfer it;
(5) Transfer the waste to a short lived storage point for medical waste along a specified route at a fixed time point and store the waste separately at a fixed location;
(6) The medical waste shall be collected and disposed of by an approved medical waste disposal provider.
7 Procedures for Taking Remedial Actions against Occupational Exposure to COVID-19
 |
Procedures for Taking Remedial Actions against Occupational Exposure to COVID-19Corona Virus || COVID -19 Protection and Treatment |
(1) Skin exposure: The skin is directly contaminated by an out sized amount of visible bodily fluids, blood, secretions or fecal matter from the patient.
(2) Mucous membrane exposure: Mucous membranes, such as the eyes and
respiratory tract are directly contaminated by visible bodily fluids, blood,
secretions or fecal matter from the patient.
(3) Sharp object injury: Piercing of the body by sharp objects that were directly exposed to the patient's bodily fluids, blood, secretions or fecal matter.
(4) Direct exposure of respiratory tract: slump of a mask, exposing the mouth or nose to a confirmed patient (1 miter away) who isn't wearing a mask.
(3) Sharp object injury: Piercing of the body by sharp objects that were directly exposed to the patient's bodily fluids, blood, secretions or fecal matter.
(4) Direct exposure of respiratory tract: slump of a mask, exposing the mouth or nose to a confirmed patient (1 miter away) who isn't wearing a mask.
8 Surgical Operations for Suspected or Confirmed Patients
8.1
Requirements for Operation Rooms and Staff
PPE
(1) Arrange the patient during a negative pressure OR. Verify the temperature,
humidity and air pressure in the operation room;
(2) Prepare all required items for the operation and use disposable surgical items if possible;
(3) All surgical personnel (including surgeons, anesthesiologists, hand-washing nurses, and charge nurses in operating room) should placed on their PPE within the buffer room before entering the operating room: Put on double caps, medical protective mask (N95), medical goggles, medical protective clothing, boot covers, latex gloves, and powered air-purifying respirator;
(4) The surgeons and therefore the hand-washing nurses should wear disposable sterile operating clothes and sterile gloves in addition to the PPE as mentioned above;
(2) Prepare all required items for the operation and use disposable surgical items if possible;
(3) All surgical personnel (including surgeons, anesthesiologists, hand-washing nurses, and charge nurses in operating room) should placed on their PPE within the buffer room before entering the operating room: Put on double caps, medical protective mask (N95), medical goggles, medical protective clothing, boot covers, latex gloves, and powered air-purifying respirator;
(4) The surgeons and therefore the hand-washing nurses should wear disposable sterile operating clothes and sterile gloves in addition to the PPE as mentioned above;
(5) Patients should wear disposable
caps and disposable surgical masks according to their situation;
(6) The charge nurses within the buffer room are liable for delivering items from the buffer area to the negative pressure operating room;
(7) During the operation, the buffer room and the operating room shall be tightly closed, and the operation must be administered as long as the operation room is under negative pressure;
(8) Irrelevant personnel shall be excluded from entering the operating room.
(6) The charge nurses within the buffer room are liable for delivering items from the buffer area to the negative pressure operating room;
(7) During the operation, the buffer room and the operating room shall be tightly closed, and the operation must be administered as long as the operation room is under negative pressure;
(8) Irrelevant personnel shall be excluded from entering the operating room.
9 Procedures for Final Disinfection
(1) Medical waste shall be disposed of as COVID-19
/ CORONA VIRUS AFFECTED related
medical waste;
(2) Reusable medical devices shall be disinfected according to the disinfection procedures of SARS-CoV-2 related reusable medical devices;
(3) Medical fabrics shall be disinfected and disposed of according to the disinfection procedures for SARS-CoV-2 related infectious fabrics;
(4) Surfaces of objects (instruments and devices including device table, operating table, operating bed, etc.);
(2) Reusable medical devices shall be disinfected according to the disinfection procedures of SARS-CoV-2 related reusable medical devices;
(3) Medical fabrics shall be disinfected and disposed of according to the disinfection procedures for SARS-CoV-2 related infectious fabrics;
(4) Surfaces of objects (instruments and devices including device table, operating table, operating bed, etc.);
G) Visible blood/bodily fluid pollutants shall be completely removed before
disinfection (handled in accordance with disposal procedures of blood and
bodily fluid spills).
All surfaces shall be wiped with a disinfectant containing 1000 mg/L active chlorine
and allowed to sit for 30 minutes with the disinfectant.
(5) Floors and walls:
G) Visible blood/bodily fluid pollutants shall be completely removed before
disinfection (handled in accordance with disposal procedures of blood and
bodily fluid spills).
All surfaces shall be wiped with a disinfectant containing 1000 mg/L active chlorine and allowed to sit for 30 minutes with the disinfectant.
All surfaces shall be wiped with a disinfectant containing 1000 mg/L active chlorine and allowed to sit for 30 minutes with the disinfectant.
(6) Indoor air: Turn off the fan filter unit (FFU). Disinfect the air by
irradiation by ultraviolet lamp for at least 1 hour. Turn on the FFU to purify
the air automatically for at least 2 hours.
10 Procedures for Handling Bodies of Deceased Suspected or Confirmed Patients
(1) Staff PPE: The staff must make
sure they are fully protected by wearing work clothes, disposable surgical
caps, disposable gloves and thick rubber gloves with long sleeves, medical
disposable protective clothing, medical protective masks (N95) or powered air
purifying respirators (PAPRs), protective face shields, work shoes or rubber
boots, waterproof boot covers, waterproof aprons or waterproof isolation gowns, etc.
(2) Corpse care: Fill all openings or wounds the patient may have, like mouth, nose,
ears, anus and tracheotomy openings, by using cotton balls or gauze dipped in
3000-5000 mg/L chlorine-containing disinfectant or 0.5% peroxyacetic acid.
(3) Wrapping: Wrap the corpse with a double-layer cloth sheet soaked with
disinfectant, and pack it into a double-layer, sealed, leak-proof corpse
wrapping sheet soaked with chlorine containing disinfectant.
(4) The body shall be transferred by the staff within the isolation ward of the hospital via the contaminated area to the
special elevator, out of the ward then directly transported to a specified
location for cremation by a special vehicle as soon as
possible.
(5) Final disinfection: Perform final disinfection of the ward and the elevator.
possible.
(5) Final disinfection: Perform final disinfection of the ward and the elevator.
V. Digital Support for Epidemic Prevention and Control Reduce the Risk of Cross Infection when Patients Seek Medical Care
(1)
Guide the general public to urge access to non-emergency services like chronic
diseases Treatment of Corona Virus Affected
on line so as to decrease the number of visitors in healthcare facilities.
Doing so minimizes the risk of cross infection.
(2)
Patients who must visit healthcare facilities should make a meeting through
other means, including Internet portals, which provide necessary guidance in
transportation, parking, arrival time, protective measures, triage information,
indoor navigation, etc. Collect comprehensive information online by patients
beforehand to enhance the efficiency of diagnosis and Treatment of Corona Virus Affected and limit the duration of the
patient's visit.
(3)
Encourage patients to take full advantage of digital self-service devices to
avoid contact with others so as to lower the risk of cross infections.
11 Lower Work Intensity and Infection Risk of Medical Personnel
(1)
Collect shared knowledge and knowledge of experts through remote consultation
and multidiscipline team (MDT) to offer the optimum therapeutics for difficult
and complicated cases.
(2)
Take mobile and remote rounds to lower unnecessary exposure risks and work
intensity of medical personnel while saving protective supplies.
(3)
Access the patients' latest health conditions electronically through health QR
codes (note: most are required to get a GREEN code through the health QR system
to travel around the city) and online epidemiological questionnaires in advance
to provide triage guidance to the patients, especially those with fever or
suspected cases, while effectively preventing the risk of infection.
(4)
Electronic health records of patients in fever clinics and therefore the CT
imaging Al system for C0VID-19 can help reduce the work intensity quickly
identify highly-suspected cases and avoid missed diagnoses.
12 Rapid Response to Emergency Needs of COVID-19 / CORONA VIRUS AFFECTED Containment
(1)
Basic digital resources required by a cloud-based hospital system allows for
immediate usage of the knowledge systems needed for emergency response to the
epidemic, such as the digital systems equipped for newly established fever
clinics, fever observation rooms and isolation
wards.
(2)
Utilize the hospital data system supported the web infrastructure frame to conduct
online training for healthcare workers and one-click deployment system, and to facilitate
the operation and support engineers to perform remote maintenance and new functions
update for medical care.
[
FAHZU lnternert + Hospital - A Model for Online Healthcare l
Since
the outbreak of COVID 19, FAHZU Internet+ Hospital quickly shifted to provide
online healthcare through Zhejiang's Online Medical Platform with 24-hour free
on line consultation, providing telemedicine service to patients in China and
even round the world.
Patients
are provided access to the first-rate medical services of FAHZU reception ,
which reduces the probabilities of transmission and nonsocial infection as a
results of their visits to the hospital. As of March 14, over 10,000 people
have used the FAHZU Internet+ Hospital online service.
•
Instructions for Zhejiang Online Medical Platform:
G)
Download Alipay app;
@
Open Alipay (China Version) and find "Zhejiang Provincial Online Medical
Platform”;
®
Choose a hospital (The First Affiliated Hospital, Zhejiang University School of
drugs);
@)
Post your question and await a doctor to respond;
® A
notification will crop up when a doctor replies. Then open Ali pay and click on
Friends;
®
Click Zhejiang
Online Medical Platform to ascertain more
details and begin your consultation. [
Establishing the International doctor Communication Platform of the first Affiliated Hospital, Zhejiang
University School of medicine.
Due
to the spread of the COVID-19 / CORONA
VIRUS AFFECTED epidemic, the first
Affiliated Hospital, Zhejiang University School of medicine
(FAHZU) and Alibaba jointly
established the International Medical Expert Communication Platform of FAHZU
with an aim to reinforce the quality of care and Treatment of Corona Virus and promote the sharing of worldwide
information resource. The platform allows doctors everywhere the planet to
attach and share their invaluable experience within the fight against COVID-19 / CORONA VIRUS AFFECTED through instant messaging with real-time translation,
remote video conferencing, etc.
•
Instructions on the International doctor Communication Platform of the first Affiliated Hospital, Zhejiang University School of Medicine
 |
Affiliate Program form Corona Virus || COVID -19 Protection and Treatment |
G)
Visit www.dingtalk.com/en to download DingTalk app.
@Sign
up together with your personal information (Name and Phone Number) and log in.
®
Apply to hitch the International doctor Communication Platform of FAHZU:
Method
1: Join by team code. Select "Contacts" > "Join Team"
> "Join by Team
Code"
, then enter the Input ID: 'YQDKl 170'.
Method
2: Join by scanning the QR code of the International doctor Communication Platform
of FAHZU.
@) Fill
out your information to hitch. Enter your name, country and clinic. ®Join the
FAHZU group chat after the ad min has approved.
®
After joining the group chat, medical staff can send instant messages assisted
byAl translation, receive remote video guidance, and access to medical Treatment of Corona Virus Affected guidelines.